Plavix: Where do we go next?
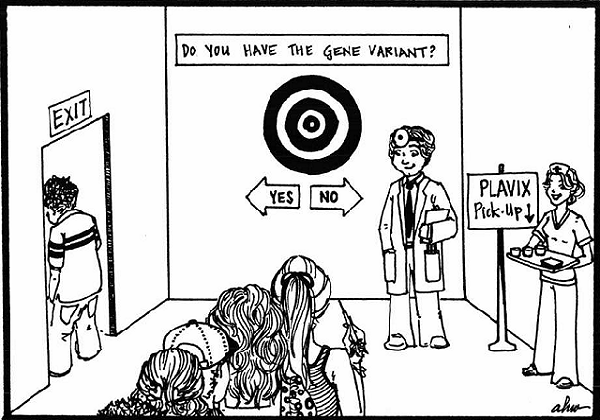
Plavix is prescribed for more than 25 million people globally and generates in excess of $9 billion dollars in annual sales. Yet, neither the U.S. Food and Drug Administration (FDA), nor the American Heart Association can provide definitive guidance to physicians for determining which patients that need antiplatelet therapy should take Plavix (or clopidogrel, the generic version of Plavix).
The problem lies with the gene variants in the CYP2C19 drug metabolizing enzyme, which occur in 1/3 of the population (Cucasians-30%; African Americans-40%; and East Asians 55%). (Desta et al. 2002). These gene variants can place patients who are taking Plavix at increased risk for having life threatening, drug-related, adverse events. However, an adverse event in these patients cannot be predicted conclusively. The reason for this is because gene variants will interact with environmental factors and other variables (including gender and other gene variants) to cause their specific effect.
A U.S. large population-based study would have the statistical power and the protocol standardization required for scientists and physicians to obtain the evidence-based data they need to address this problem.
The problem: Patients who are prescribed Plavix and have gene variants in the CYP2C19 drug metabolizing enzyme, have loss of drug metabolizing enzyme function. This loss of function has been associated with an increased risk of death, myocardial infarction, or stroke, especially among patients undergoing percutaneous coronary intervention (PCI)” (Simon et al. 2009). In one study, individuals with at least one CYP2C19 reduced-function allele (approximately 30% of the study population), had a relative reduction of 32.4% in plasma exposure to the active metabolite of Plavix, as compared with individuals without the gene variant (Mega et al. 2009). Insufficient plasma exposure means that there are fewer Plavix drug metabolites available to bind to the adenosine diphosphate receptor (ADP) in order to prevent platelet activation, which is the job Plavix is designed to accomplish.
In another study, patients with two copies of the CYP2C19 gene variant had worse clinical outcomes when treated with clopidogrel after acute myocardial infarction when compared to patients with only one copy of the gene variant (Freedman and Hylek 2009). (We receive two copies of each gene, one from each parent. Two copies of a gene variant can increase its affect.)
Because there is no evidence-based clinical strategy for prescribing Plavix, Dr. Dan Roden, MD and Dr. Alan Shuldiner, MD published an editorial in the July 27th, 2010 NEJM, in which they reviewed the following options available for physicians who must prescribe antiplatelet inhibitors:
- Do nothing; follow guidelines:
The authors suggest this as a tenable choice in the absence of availability of any other solid data or testing (Roden and Shuldiner 2010).
- Use platelet function testing as an alternative, or in combination with, CYP2C19 genetic testing:
The scientists noted that platelet function testing lacks standardization. Specifically, there are inconsistent results between different platelet assays to identify clopidogrel non-responders. Many patients who are identified as non-responders with one test, are identified as good responders with other tests (Cuisset et al. 2010).
Nonetheless, the authors suggest that there may be benefits to combining platelet function monitoring and genetic CYP2C19 genetic testing to manage P2Y12 inhibitor therapy. They state that CYP2C19 genotyping testing would allow physicians to identify patients at higher risk for clopidogrel failure. Furthermore, intermittent platelet function testing would allow the clinician to address the variance in drug action while, at the same time, factoring in the CYP2C19*2 results (Roden and Shuldiner 2010).
- Use prescription genotyping to guide therapy:
According to the authors, this option does not have evidence-based support. The authors note that because many cardiovascular events occur within the first few hours to days after percutaneous coronary intervention, a rapid turnaround time is essential. According to the authors, “The questions here are how and whether to adjust clopidogrel dose, or to choose an alternative drug; and in whom: just poor metabolizers (*2/*2 homozygotes) or also in intermediate metabolizers (*1/*2 heterozygotes)? In addition, third-party payers may or may not reimburse for genetic testing without the evidence base to support its efficacy” (Ibid).
- “Ignore clopidogrel and prescribe “alternate P2Y12 receptor inhibitors” (i.e., prasugrel for now) to all”:
The authors point out that for now, the alternative platelet inhibitor “Prasugrel,” from Daiichi Sankyo Co Ltd and Eli Lilly and Co., does not appear to be adversely affected by CYP2C19 polymorphic genotype. They also cite data from the Optimizing Platelet Inhibition With Prasugrel-Thrombolysis in Myocardial Infarction 28 (TRITON-TIME 38) study, showing that “Prasugrel resulted in fewer cardiovascular adverse events in patients, but more bleeding.”
Hence, the authors note that giving Prasugrel to all patients would eliminate the need for CYP2C19 gene variant genotyping, but it would also increase “exposure to adverse bleeding complications” (Ibid).
- Prescribe clopidogrel in patients without at-risk genotypes and other drugs, such as prasugrel, in subjects with CYP2C19 variant genotypes:
The authors suggest that, to increase the “benefit to risk ratio,” and to also manage health care costs, a more individualized approach might be to prescribe clopidogrel in patients who don’t have at-risk genotypes and prescribe other drugs such as “prasugrel” in subjects with CYP2C19 variant genotypes. “This option might also be cost effective, with clopidogrel coming off patent in 2011, and soon to be much less expensive than newer agents. However, as the American College of Cardiology Foundation/American Heart Association Clopidogrel Clinical Alert correctly points out, the evidence-base for this option currently does not exist.” (Ibid)
Finally the authors state that, “clearly none of these options are well supported by data and that major issues are unsettled: e.g., which platelet function test is best, how to get timely genetic data on which to act, how to act, and the economics of genetic testing versus complications avoided” (Ibid).
These options must echo the frustration that many physicians share.
The fault, for this lack of guidance for prescribing Plavix does not lie with regulatory agencies, nor does it lie with physicians. Regulatory agencies, as well as physicians, have been informed by the excellent scientific studies that have been conducted since 2007, to understand how the CYP2C19 drug metabolizing enzyme polymorphisms affect the potential for adverse events in diverse patient population subsets that are prescribed Plavix.
However, these clinical studies could not have taken into account all of the factors that scientists suggest could contribute to the gene variant’s causal role in adverse drug related events. For example:
- Numerous environmental factors, specific to an individual’s geographical region, may combine with a gene variant to influence adverse drug events.
- Other gene variants may interact with the CYP2C19 gene variant and affect the outcome of Plavix or other antiplatelet inhibitors such as Prasugrel.
- A patient’s ancestral admixture, which reflects the differing proportion of individual genes that a person inherits from his ethnic ancestry, may affect the degree of clinically relevant adverse drug events.
- Newly discovered small molecules that can participate in affecting protein expression patterns along drug metabolizing relevant, cellular signaling pathways, could influence Plavix outcome, such as micro RNAs (miRNAs).
- New, rare gene variants may also influence clinically relevant outcomes for patients who are prescribed Plavix, and more of these are expected to be discovered as novel, Third Generation DNA Sequencing Platforms enter the marketplace.
In short, a fundamentally new genetic science is being incorporated into the health care decision-making paradigm and it is changing our conceptual framework about medical practice.
The U.S. Government made a $3 billion dollar investment to decode the human genome, in order to bring this about. In their planning, scientists, physicians, and legislators knew that this genetic data would have the potential to introduce changes within the very fabric of our health care infrastructure. However, it was difficult to anticipate what the timing and the exact nature of those changes would be. Now scientists have better information to work with. Specifically, they know that they have diverse sets of genomic data that must be cross referenced and analyzed in what Gregory Feero, Alan Guttmacher, and Francis Collins, in a recent NEJM article, described as, “a longitudinal living laboratory,” operating across the nation (Feero, Guttmacher and Collins 2010).
Such a living laboratory would serve to help scientists and physicians elucidate the relationship between adverse drug responses, and an individual’s genetic make-up.
As Feero, Guttmacher and Collins noted in their article, the amount of genetic data available is enormous and it is still growing. “The wealth of scientific discovery generated over the past 10 years is unparalleled in the history of biomedicine. Moreover, the rate of discovery is accelerating” (Feero et al. 2010).
Hence, the U.S. Health Care Infrastructure is at a unique juncture. The situation requires that the U.S. Health Care System design a new personalized medicine component that will enable a dynamic, multidiscipline team to conduct a large population-based study spanning multiple regions across the nation. Such a study might include more than a million people in its design.
This type of study will provide the statistical power, and protocol standardization necessary, to arrive at clinical strategies for evidence-based medical decisions that will incorporate patient genotypes.
Today, scientists and physicians at different locations across the nation are working on different aspects of personalized medicine and health care system components that could possibly become part of a larger system design. One goal might be to bring these scientists and physicians together with their regional counterparts, to create a collaborative venture and work as a team to expand the design, development and implementation of these system components across the nation.
For example, Marylyn Ritchie and her colleagues at Vanderbilt University School of Medicine, in Nashville, TN, recently published an article describing a study they completed. The study demonstrated that the Vanderbilt DNA repository data bank, “BioVu,” could be successfully linked to their electronic medical records database, in order to generate large numbers of “subjects.” These subjects could then be used as both “cases” and “controls,” across multiple diseases, in studies to be conducted by scientists and physicians (Ritchie et al. 2010).
Today, scientists and physicians at different locations across the nation are working on different aspects of personalized medicine and health care system components that could possibly become part of a larger system design.
The important work done by these scientists could create a model for linking electronic medical records to DNA repositories, in order to augment or supplement traditional research designs that enroll cases and controls prospectively, while at the same time systematically collecting relevant phenotype (physical expression) data. Such a system would accommodate a statistically powerful, large population-based study that could be implemented in regions across the nation.
In a second example, Cathy Schaefer, Ph.D, and Neil Risch, Ph.D., are co-directing a research program on “Genes, Environment, and Health,” that will support the genome-wide analyses of DNA samples from 100,000 Kaiser Permanente members.
To accomplish this, Kaiser Permanente will use Affymetrix’s “Axion Genomics Solution” on the Gene Titan Microarray Platform to genotype these patients. Permanente will use the genotype data to discover which genes, in combination with environmental factors (such as the air we breathe, the water we drink, the food we eat, and our lifestyles and habits), are linked to specific diseases and their onset and progression, as well as to adverse drug events.
This new and detailed genetic information, which for the first time is being generated on such a large and diverse population, will be linked to decades of historical, clinical and other health-related information on these study participants, that will be obtained from health surveys contained in the Kaiser Permanente electronic health records. This data can then be used by physicians to design strategies to help their patients delay and/or prevent disease onset. Furthermore, it can be used to determine if these strategies are working. This patient genotype data will also be used by physicians to better understand what drugs might produce an adverse reaction in their patients and design strategies to prevent them.
The Kaiser Permanente program may be well suited as a model for a second component of a U.S. large population-based study that could operate regionally across the nation. This would include the analysis of environmental factors in combination with gene variants in order to understand how potential adverse drug events occur.
Risch, who also holds positions in Genetics and Epidemiology at the University of San Francisco (UCSF), in CA, has also worked with his colleagues at UCSF to study and incorporate ancestral admixture data into genotyping analysis. Hence, this newly emerging aspect of genotyping will most likely be accounted for in the program under development by Kaiser Permanente.
These are only two examples of programs that can be used as models for a U.S. Regional Health Care Infrastructure that could include a personalized medicine division, with the requisite system components in place to launch a Large Population-Based Study.
I am sure there are also other models of workable system components under development within organizations at other locations across the U.S.
Moving forward to implement this concept, one might start by identifying these organizations to find out if they would consider bringing their works-in-progress into a collaborative format.
Importantly, such a collaboration among organizations like Vanderbilt, Kaiser Permanente, and the University of California at San Francisco, with select regional health care centers around the country, would enable the U.S. to be one step further along in its vision for conducting a Large Population-Based Study, that informs the growth of evidence-based decision making in personalized medicine across the United States.
Accomplishing this goal was explored in a report that was delivered to the U.S Health and Human Services (HHS) Secretary in 2007, by the Secretary’s Advisory Committee on Genetics, Health, and Society (SACGHS).
A key finding in the report supported the creation of a Large Population Based Study (LPS). According to the Report:
On the basis of the knowledge gathered… the committee believes that a new LPS in the United States could lead to improved diagnostics, treatments and preventative measures for common diseases such as cardiovascular disease, diabetes, and cancer.
Hence, a Large Population Based study may be what is next as an option that supports evidence-based medicine for physicians.
References:
-
Cuisset, T., C. Frere, R. Poyet, J. Quilici, B. Gaborit, L. Bali, O. Brissy, M. Lambert, P.-E. Morange, M.-C. Alessi & J.-L. Bonnet (2010) Clopidogrel response: Head-to-head comparison of different platelet assays to identify clopidogrel non responder patients after coronary stenting. Archives of Cardiovascular Disease, 103, 39-45.
-
Desta, Z., X. Zhao, J.-G. Shin & D. A. Flockhart (2002) Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clincal Pharmacokinetics, 41, 913-958.
-
Feero, W. G., A. E. Guttmacher & F. S. Collins (2010) Genomic Medicine – An Updated Primer. NEJM, 362, 2001-2011.
-
Freedman, J. E. M. & E. M. M. Hylek (2009) Clopidogrel, Genetics, and Drug Responsiveness. New England Journal of Medicine, 360, 411-413.
-
Mega, J., S. Close, S. Wiviott, L. Shen, R. Hockett, J. Brandt, J. Walker, E. Antman, W. Macias, E. Braunwald & M. Sabatine (2009) Cytochrome P450 genetic polymorphisms and the response to prasugrel: relationship to pharmacokinetic, pharmacodynamic, and clinical outcomes. Circulation, 119, 2553-60.
-
Ritchie, M., D. , J. C. Denny, D. C. Crawford, A. H. Ramiez, J. B. Weiner, J. M. Pulley, M. A. Basford, K. Brown-Gentry, J. R. Balser, D. R. Masys, J. L. Haines & D. M. Roden (2010) Robust Replication of Genotype-Phenotype Associations across Multiple Diseases in an Electronic Medical Record. The American Journal of Human Genetics, 86, 560-572.
-
Roden, D. M. & A. R. Shuldiner (2010) Responding to the Clopidogrel Warning by the US Food and Drug Administration. Real Life Is Complicated. Circulation, 122.
-
Simon, T., C. Verstuyft, M. Mary-Krause, L. Quteineh, E. Drouet, N. Meneveau, P. G. Steg, J. Ferrieres, N. Danchin & L. Becquemont (2009) Genetic Determinants of Response to Clopidogrel and Cardiovascular Events. New England Journal of Medicine, 360, 363-375.